We represent dozens of police officers, firefighters, and other first responders who have developed post-traumatic stress disorder (PTSD) due to work-related traumatic events.
PTSD is a serious, sometimes debilitating mental illness that can wreak havoc on a person’s family, social, and work life. Fortunately, things can get better with time and treatment.
The “best” type of treatment for PTSD varies from person to person and can be used individually or in combination with other treatment modalities.
What Is Post-Traumatic Stress Disorder?
Post-traumatic stress disorder (PTSD) is a mental health condition that may develop in people who experience one or more traumatic events. While anyone can develop PTSD, it manifests more often in veterans, victims of sexual assault, victims of domestic violence, and, as we’ll be discussing today, first responders.
PTSD stems from maladaptations in our body’s natural survival mechanisms, which are controlled by the amygdala, often called the “fear center” of the brain.
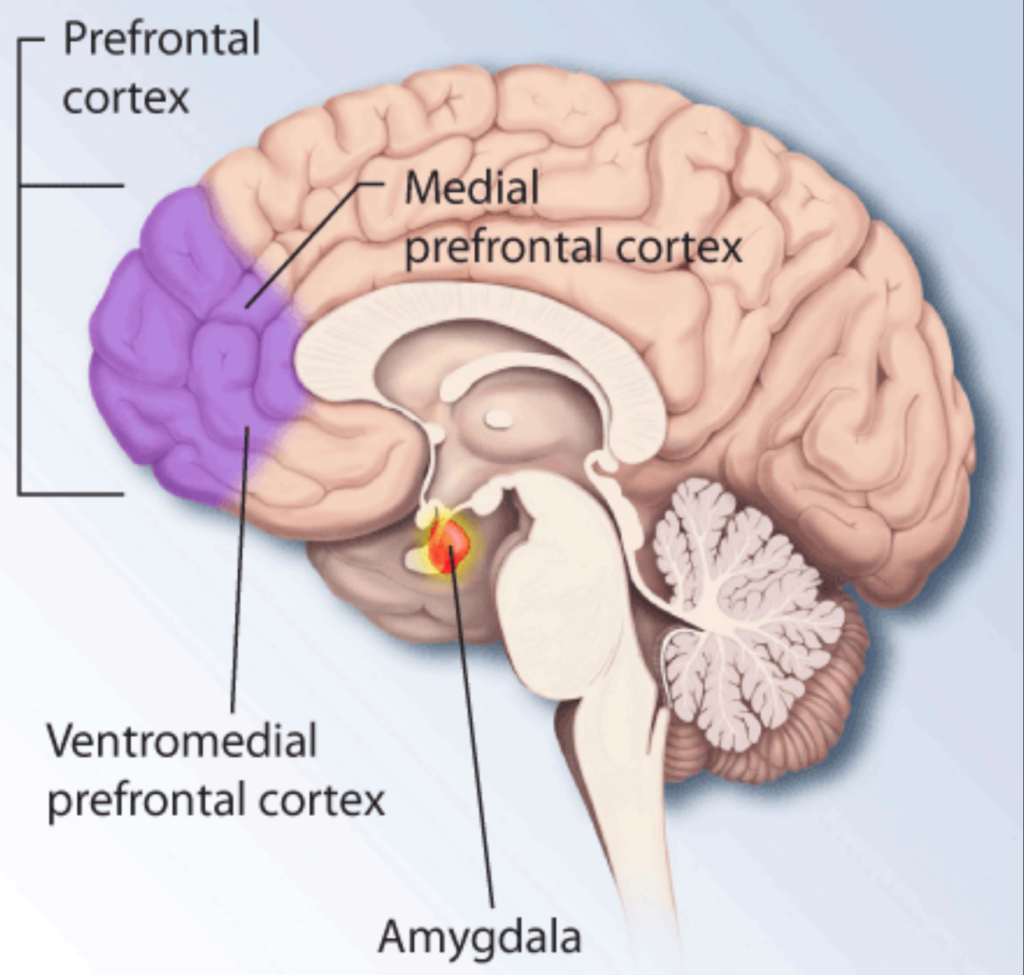
When the amygdala activates, it kicks the body into fight or flight mode, causing a rush of stress hormones like adrenaline and cortisol. As they flood the brain and body, we experience a temporary boost to our senses and reflexes. Cortisol, in particular, even increases blood sugar levels so the muscles have enough energy to act quickly to escape the danger as soon as possible.
While this sudden flood of hormones is helpful when someone is in an actual survival situation, sometimes the brain and body struggle to reset after a traumatic event is over. Instead, they continue to produce stress hormones as if they were in a survival situation, leading to PTSD symptoms like anxiety and hypervigilance.
The Long-Term Consequences of Untreated PTSD
Over time, people with PTSD can experience worsening symptoms as the overabundance of stress hormones deteriorates the prefrontal cortex, which controls reasoning and decision-making, and the hippocampus, responsible for memory storage and retrieval.
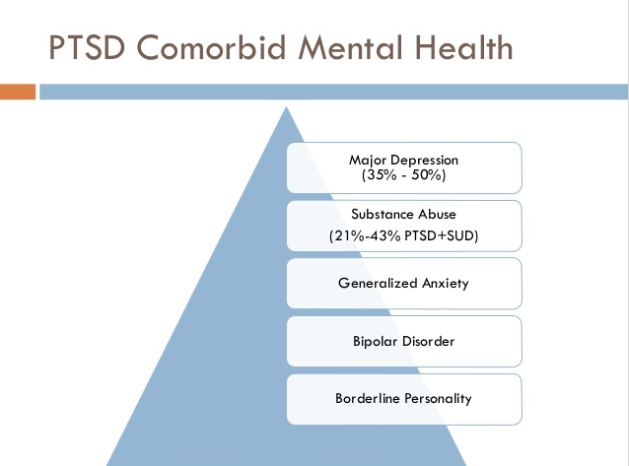
People with PTSD also tend to self-medicate with drugs or alcohol if they don’t feel that medications and therapy are working. A 2010 study called “The use of alcohol and drugs to self-medicate symptoms of posttraumatic stress disorder” found that around 20% of people with PTSD used substances to relieve their symptoms, which in turn can lead to higher suicide rates and lower quality of life.
PTSD Diagnostic Criteria
For an individual to be diagnosed with PTSD, they must meet certain criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) must be met:
- Exposure to a Traumatic Event
The individual must have been exposed to death or threatened death, serious injury, or sexual violence. This exposure could be direct, witnessed, or even indirect (such as learning a close family member or friend experienced trauma.
The trauma may also occur as a result of experiencing repeated or extreme exposure to aversive details of the traumatic event(s). The DSM-V-TR provides specific examples of indirect trauma that may be experienced by first responders, e.g., first responders collecting human remains and police officers exposed to details of child abuse.
- Persistent Re-experiencing of the Event
People with PTSD frequently relive the trauma through intrusive thoughts, nightmares, or flashbacks. They may also experience psychological distress or physical reactions to reminders of trauma. Reminders can trigger this re-experiencing or can occur spontaneously.
- Avoidance of Stimuli Related to the Event
Those with PTSD tend to avoid thoughts, feelings, conversations, activities, places, or people that remind them of the event.
- Persistent Symptoms of Increased Arousal
Symptoms include irritability, outbursts of anger, reckless or self-destructive behavior, hypervigilance, an exaggerated startle response, and difficulty concentrating or sleeping.
- Negative Alterations in Cognition and Mood
This can manifest itself as difficulties with experiencing positive emotions, overly negative thoughts about the word, feelings of isolation, memory loss regarding aspects of the traumatic event, and decreased interest in hobbies or activities.
These PTSD symptoms must last over a month and be severe enough to interfere with relationships, daily activities, or work performance.
PTSD in First Responders
First responders often work in environments that are ripe for the development of PTSD. They are routinely exposed to high-stress, high-stakes situations, whether a police officer encountering violent crime or a firefighter battling a life-threatening blaze.
This frequent exposure to severe stressors over many years can accumulate over time in a phenomenon known as “cumulative trauma,” resulting in a form of PTSD called “complex PTSD.”
Additionally, the shift work, long hours, and lack of control over assignments can exacerbate stress, making it more difficult for the body and mind to recover fully.
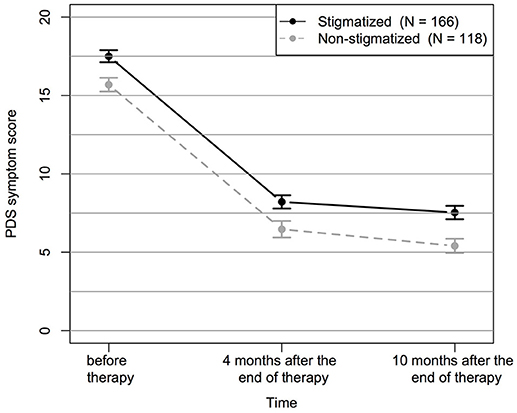
Often making the situation worse is that the culture within some first responder organizations discourages open discussion about emotional and mental health, contributing to stigma and a lack of support for those affected by PTSD.
PTSD Treatments
If you are suffering the debilitating effects of PTSD, reclaiming your life starts with finding a treatment method to help manage symptoms and process the trauma.
Cognitive Processing Therapy (CPT)
One of the more frequently used therapy options to treat PTSD is cognitive processing therapy (CPT). This approach was born out of the broader field of cognitive behavioral therapy (CBT) with the specific intention of helping manage PTSD symptoms after sexual assault. It has since grown to encompass a much wider range of patients, including first responders.
CPT treatment aims to help patients get “unstuck” by challenging how you make sense of the traumatic event and its aftermath. For example, you may believe that you are at fault or to blame for the traumatic event(s), a common thought process in those with PTSD.
Through talk therapy, a mental health professional will help you evaluate all the things that were outside of your control to move forward and accept that the event was not your fault, despite what you did or did not do, in a process called “cognitive restructuring.”
Some studies have even found that the benefits of cognitive processing therapy can extend to other areas of mental health, including reductions in symptoms of depressive disorders, panic disorder, and generalized anxiety disorder.
This type of cognitive therapy is considered a particularly beneficial treatment in people who anticipate encountering additional trauma—such as police officers, firefighters, paramedics, EMTs, nurses, or members of the armed forces. These vocations regularly place people in traumatic situations, and CPT treatment may help alter how first responders interpret and process trauma, making it easier to continue with their chosen field of work.
What Is the Process Like?
CPT typically consists of 12 weekly sessions, during which your therapist will help you understand and challenge how you make sense of your trauma by targeting “stuck” thoughts or feelings that linger in the aftermath.
During your sessions, you can expect to do the following:
- Identifying your stuck points and negative beliefs, such as “The event was my fault” or “The world is always dangerous.”
- Contradicting your stuck points by looking at alternative viewpoints and evidence that proves otherwise.
- Build skills to manage everyday stress better and avoid slipping back into old thought patterns.
- Confronting your trauma and feelings about it in a safe, supportive environment.
- Practicing what you’ve learned about cognitive processing therapy in real-world scenarios, then discussing outcomes with your therapist.
- Planning for a future where the traumatic event no longer controls your life or relationships.
How Effective Is CPT?
Statistics show that cognitive processing therapy can have a significant impact across types of trauma, with studies reporting that anywhere from 30% to 97% of people who complete their CPT treatment program no longer meet the diagnostic criteria for PTSD.
Prolonged Exposure Therapy (PET)
For many people with PTSD, avoiding trauma reminders feels like the safest thing to do. Prolonged exposure therapy (PET) challenges that idea by asking patients to take the opposite approach and face the triggers head-on.
Like CPT, it is a form of cognitive therapy but with more of a focus on easing severe phobias or comorbid anxiety disorders that often accompany PTSD. It is most frequently used in the Veterans Affairs system and has been considered intense by many of my clients who have gone through it.
PET is considered appropriate for people with unwanted thoughts, nightmares, hypervigilance, and hopelessness.
What Is the Process Like?
PET is an individual therapy between yourself and your mental health professional, lasting about 90 minutes per session, and typically is prescribed for three months or more.
During the process, you’ll work through stages that ask you to:
- Learn calming techniques, like deep breathing, to help manage anxiety during the sessions.
- Recount your traumatic experience to the therapist, who will help you confront and make sense of your memories.
- Write down your traumatic experience and read it aloud while you explore your thoughts and feelings.
- Compile a list of all the things you have been avoiding (e.g., smells, sounds, places, etc.) and rank each item based on how much distress they cause you when you encounter them.
- Gradually confront real-world situations that you’ve been avoiding but are safe.
- Discuss any remaining fears and plan how to manage any future symptoms.
How Effective is Prolonged Exposure Therapy?
Extensive research shows that prolonged exposure therapy is one of the most effective first-line treatments for PTSD symptoms, with positive outcomes in 65-80% of patients. However, there are many critics of PET because it is considered cruel and inhumane to force patients to confront their trauma in such a direct way. It also correlates with high drop-out rates, suicide rates, and instances of violence.
Stress Inoculation Training (SIT)
Stress inoculation training (SIT) is a type of cognitive behavioral therapy that equips you with a toolkit of coping strategies to manage stress and reduce symptoms of PTSD, although it is not a specialized PTSD treatment.
The fundamental idea behind SIT therapy is similar to medical inoculation. By exposing individuals to manageable amounts of stress in a controlled environment, they can build psychological resilience to handle more significant stressors.
What Is the Process Like?
Typically, you will not have to go into detail about your traumatic experiences while doing SIT treatment. It’s also typically available as group therapy if you’re uncomfortable with the idea of individual therapy.
Over the course of 8 to 15 sessions, you’ll work to:
- Learn about stress and its effects on the mind and body.
- Practice coping skills like deep breathing techniques, muscle relaxation, and positive self-talk.
- Apply new coping mechanisms in simulated stressful scenarios.
- Take your coping mechanisms to the real world, then discuss them with your support group or therapist.
- Reinforce your new learnings and learn how to maintain them going forward.
How Effective is Stress Inoculation Training?
Most data shows that while SIT can be effective on its own, it’s more effective when combined with other treatments like PET, which has a 40-60% rate of participants experiencing symptom improvement to the point that they no longer have a PTSD diagnosis.
Eye Movement Desensitization and Reprocessing (EMDR)
Eye movement desensitization and reprocessing (EMDR) is a psychotherapy that helps patients process trauma from a more bodily-focused approach.
Unlike talk therapy, EMDR therapy does not rely on going through your traumatic experiences with your therapist.
Instead, you concentrate on an event while you watch something your therapist is doing, such as rapidly moving a hand, finger, or a light back and forth. As you follow this movement with your eyes, the swift eye movements loosen the knots in your memory and allow negative thoughts and memories to be reprocessed in a more neutral way.
What Is the Process Like?
In most cases, EMDR treatment requires about three months of sessions to be effective. There is some controversy surrounding the efficacy of EMDR; however, you will typically know whether this type of treatment plan will work for you after one session.
Generally, an EMDR treatment plan progresses as such:
- Learn self-control techniques for managing emotional distress as you start processing the trauma.
- Identify target memories to focus on and any negative beliefs, emotions, or bodily sensations associated with them.
- Desensitize yourself to the trauma by focusing on the traumatic memory while the therapist guides your eyes in a specific movement pattern until the memory becomes less distressing.
- Install positive beliefs to replace the negative ones, like replacing a feeling of hopelessness with a sense of empowerment.
- Work through a body scan by noting any physical tension or discomfort when recalling the traumatic event, then process these physical sensations with more eye movement desensitization.
- Come back to equilibrium at the end of sessions so you leave feeling stable and grounded.
How Effective is EMDR?
As a trauma therapy, EMDR has grown in popularity recently as more data emerges showing its effectiveness.
In 70% of studies, EMDR therapy was more rapid and effective than trauma-focused CBT. Various other randomized controlled trials have shown that 77-91% of patients no longer qualify for a PTSD diagnosis at their follow-up appointment after 3-8 sessions.
Accelerated Resolution Therapy (ART)
Accelerated Resolution Therapy is a newer type of psychotherapy and shares many of the same characteristics of cognitive behavioral therapy and EMDR. As the name implies, it’s also an accelerated approach to post-traumatic stress disorder treatment that directly addresses trauma and related emotions.
Trauma-focused ART aims to process traumatic memories and images associated with traumatic situations and reprogram the way they are stored in the brain so that they no longer trigger strong emotional and physical reactions. A therapist will have you visualize the experienced trauma and perform specific eye movements.
As you do so, your therapist will encourage you to replace traumatic images with positive or neutral images to desensitize you to the event and help you gain control over your emotional response when thinking about it.
What Is the Process Like?
The ART process is intended to be fast, often completed within one to five sessions, each lasting 60 to 75 minutes.
Here’s what you can generally expect:
- Learn imagery and relaxation techniques, such as deep breathing.
- Identify target memories or images that trigger your symptoms.
- Follow directed eye movements while focusing on these memories to keep your brain activity engaged in a way that allows you to process the memory more effectively.
- Re-script or replace the memory with a more positive or neutral outcome by visualizing a new narrative or image to replace the distressing one.
- Identify and process physical sensations related to traumatic memories.
- Return to a relaxed state and discuss the changes you’ve noticed to determine if more sessions are needed.
How Effective Is ART?
Because it is still an emerging treatment, ART doesn’t have as robust a field of study as more traditional treatment options. Early data shows promise, though, with a 61% positive response rate and a needed-session rate of 3.7 ± 1.1, much lower than the 8-15 sessions needed for other treatments.
Medication
In conjunction with the treatment modalities discussed above, many people with post-traumatic stress disorder also take medications to help manage their psychological symptoms.
The FDA has approved only the selective serotonin reuptake inhibitors (SSRIs) paroxetine and sertraline as specialized treatments for treating PTSD. Still, there are many other medications out there that have been deemed effective in relieving symptoms.
These medications may include:
- Antidepressants
- Monoamine oxidase inhibitors (MAOIs) allow your brain to “hold on to” more of the neurotransmitters serotonin, dopamine, and norepinephrine by inhibiting a chemical called monoamine oxidase.
- First-generation antipsychotics (FGAs) slow down dopamine activity by blocking their receptors. They are less commonly used because of the severe side effects, including involuntary movements, sedation, and an altered mental state.
- Second-generation antipsychotics (SGAs) are very similar to FGAs, but don’t affect dopamine levels to the same extent. Rather, they affect several neurotransmitters, like serotonin, to reduce the risk of side effects associated with chronically low dopamine levels.
- Beta-blockers, or beta-adrenergic blocking agents, are usually used to treat high blood pressure, but their mechanism of blocking the effects of the hormone epinephrine (adrenaline) can reduce the physical symptoms of PTSD by lowering the heart rate.
- Benzodiazepines are extremely powerful anti-anxiety and muscle relaxant medications. They work to enhance the effects of the neurotransmitter gamma-aminobutyric acid (GABA), which is responsible for slowing down brain activity. They are a sedative and can help manage PTSD-related insomnia. However, their addictive properties can be very dangerous if taken long-term. The US Department of Veterans Affairs recommends against their use in PTSD treatment.
After starting one of these medications, your doctor will schedule a follow-up appointment to see how it’s working. Be 100% honest during this conversation. Some side effects are normal, depending on the medications, while others could lead to much more significant issues if not dealt with.
Final Thoughts
All of the PTSD treatments discussed here have been found to be effective. The “right” treatment plan will vary from person to person and what he or she is comfortable with. If your symptoms persist, then you may consider whether it is in your best interest to continue in the profession.Once first responders stop working, they are no longer exposed to the constant triggers of their jobs. This allows them time to heal, get professional help, and move forward.
If you or someone you know suffers from PTSD due to a work-related traumatic events, you should consult with an experienced attorney in this area of the law. At Meuser Law Office, P.A., we have represented many clients with PTSD, including police officers, firefighters, correctional officers, 911 dispatchers, EMTs, paramedics, ER and trauma nurses, and other first responders. We understand this nuanced area of the law and work with our client to ensure you receive the full benefits to which you are entitled. Contact Meuser Law Office, P.A. for a no-obligation consultation today. Call us today at 952-345-2052.